21 October 2020
Article from October INPractice
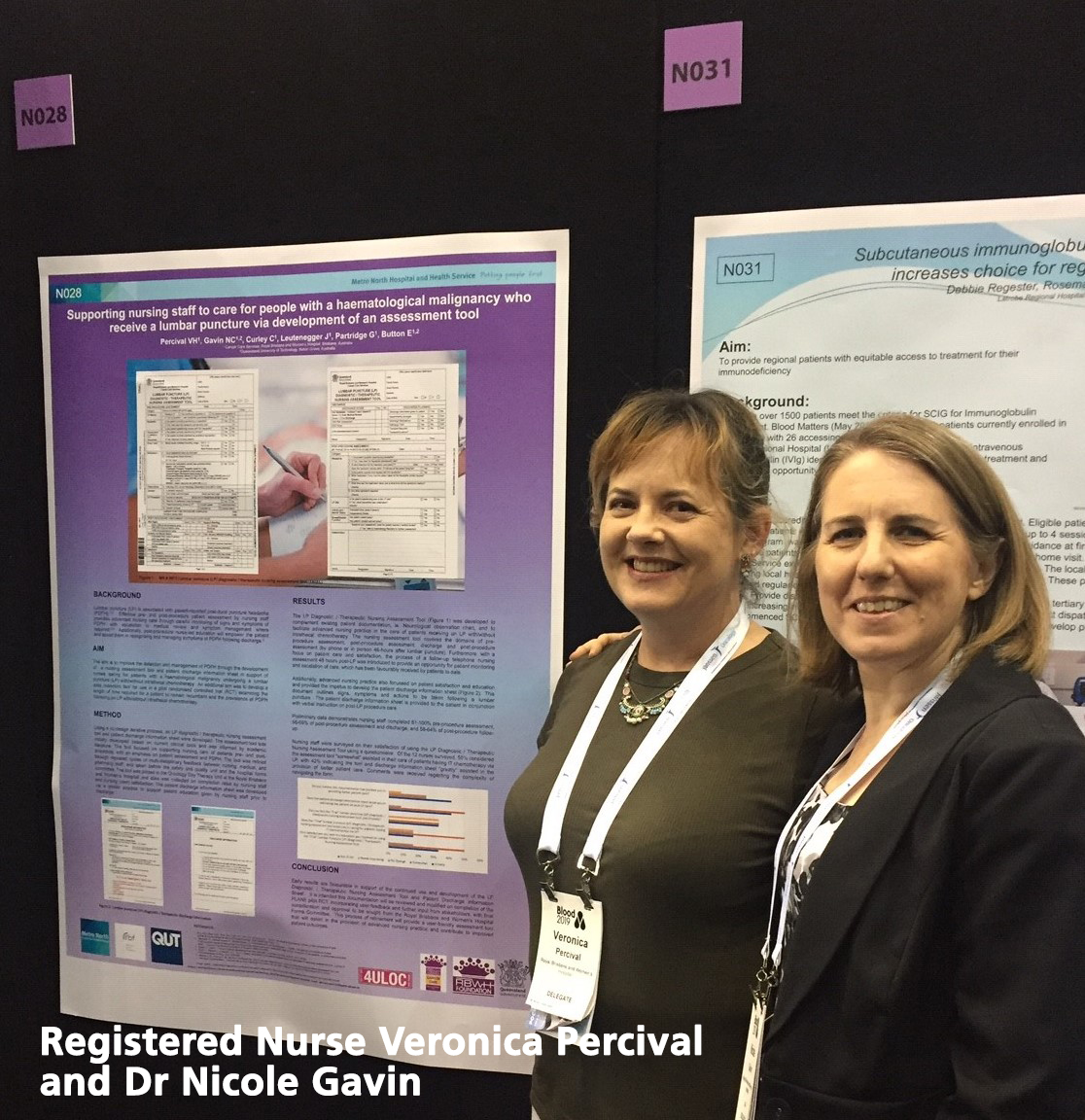
Two nurses are leading a research push to make cancer patients' lives that little bit more comfortable.
Dr Nicole Gavin, who runs a ground breaking Nursing Research Internship, and Registered Nurse Veronica Percival are piloting an innovative trial in haematology patients who require a lumbar puncture for the diagnosis and treatment of their haematological malignancy (blood cancer).
The most commonly diagnosed blood cancers are non-Hodgkin lymphoma, chronic lymphocytic leukemia, acute myeloid leukemia, acute lymphoblastic leukemia and multiple myeloma.
It is not currently clear if time spent lying flat following a lumbar puncture impacts the development of a post-dural puncture headache (PDPH) or its severity - but Dr Gavin and Registered Nurse Percival now have the funds to investigate the link, thanks to a $25,000 grant from the Adelaide-based Rosemary Bryant Foundation.
The Rosemary Bryant Foundation aims to strengthen the role of the nursing and midwifery professions through the development of a research-driven, evidence-based platform of health care, such as the lumbar puncture trial.
Named after Rosemary Bryant AO, Australia first Commonwealth Chief Nurse and Midwifery Officer, Emerita Director of Nursing at the RAH and honorary Iife member of the ANMF (SA Branch), the Foundation ultimate aim is to create a more informed and productive workforce that can provide optimal care to the community. The Foundation seeks applications for high-quality research projects which have a strong focus on being able to be translated into practice.
The results of Dr Gavin and Nurse Percival pilot study will be the basis of an application for additional funding for a multi-site randomised controlled trial which will provide equitable and quality nursing care. The results of this study might be transferable to other populations that require a lumbar puncture.
"A lumbar puncture is a procedure that many oncology nurses are familiar with," Ms Percival says.
"It is the procedure whereby a needle is inserted into the lower back to reach the cerebrospinal fluid that sits around the spinal cord. It is conducted for both diagnostic and therapeutic purposes such as intrathecal chemotherapy."
Although effective, Ms Percival says the procedure is unfortunately associated with post-dural puncture headaches, which can be debilitating. Other symptoms include neck stiffness, tinnitus, reduced hearing, sensitivity to light and nausea. The headaches can last from days to weeks following the procedure.
"Our study will compare patients lying flat for one hour versus two hours following a lumbar puncture with or without intrathecal chemotherapy in the hope of determining a relationship between POPH and length of time lying down following the procedure," she says.
Reducing time spent lying flat will benefit the patient, free up hospital resources (i.e., beds) and improve patient flow through outpatient departments.
The study will also seek to promote nursing care and patient satisfaction by supporting advanced practice nursing with a specialised nursing assessment tool for use before and after the lumbar puncture. In addition, prior to discharge, postprocedure education and printed discharge information will be given to the patient by their nurse, providing instruction on care following their lumbar puncture.
To assess the effectiveness of this intervention, patients will be called 48 hours following the lumbar puncture for a nursing assessment and asked to complete a satisfaction survey one month later.
"We have found that the patients have been very receptive to the follow-up phone call," Ms Percival said. "They've always been very happy to receive a phone call. "The questions we ask patients 48 hours after ... have they experienced a headache? If so. how would they rate the pain.
"What medications did they take?
Did that medication help?
"Were there any other symptoms to report like nausea, vomiting?
"Whether the bowels have opened and are voiding within that time. Whether they are able to mobilise independently."
"We're looking at neurological issues as well," Dr Gavin said. We assess whether people are able to communicate coherently.
"Should they have any concerns we can escalate it through to a clinician or have them come in to be reviewed .. so it's just that extra point in safety for these patients.
"I think people often see how busy we are in hospitals and they don't want to ring up and bother us and so this is really a way of circumnavigating that."
Dr Gavin and Ms Percival aim to recruit 110 patients, with the results originally due last August.
"At this moment things are going ahead but we can't predict how many lumbar punctures are going to be done ... due to the COVID19 pandemic," Ms Percival said.
Dr Gavin, a Registered Nurse originally from England, is a Master of Advanced Practice (Health Care Research) and a Doctor of Philosophy who alternates between the Royal Brisbane and Women's Hospital and the Centre for Healthcare Transformation, Queensland University of Technology. Winne, of Best Research Paper (Cancer Nurses' Society Australia Congress 2018) and Best PhD student (2017; with research into the effect of parenteral nutrition on microbial growth and its influence on catheter-related infection in patients with a central venous access device), Or Gavin is highly considered by her colleagues to be a potential world-leader in nursing research.
Ms Percival is a Bachelor of Nursing graduate and Registered Nurse since 2011 and is currently being mentored by Dr Gavin as a clinical researcher, in haematology and medical oncology.
In addition to pursuing her own early career research, Dr Gavin is instrumental in providing research support to about 250 registered nurses in Cancer Care. She offers a 12-week Evidence Based Practice Programme and a 12-month Nursing Research Internship.
The registered nurses enrolled in this programme present their work at local and national conferences and will be publishing their results in peer-reviewed journals. This experience gives registered nurses the confidence to enrol in a postgraduate degree. Currently 26% of registered nurses in Cancer Care Services, Royal Brisbane and Women's Hospital have a postgraduate qualification or are enrolled and the aim is to increase postgraduate enrolments.
"We've got frontline nurses leading multi disciplinary research. They're taking clinical questions and turning them into fundable research studies, Dr Gavin says.
"I think we're one of the only models in the country that offers this support, so we're very proud of our internship and how we teach research to our frontline staff."
The Research Internship Programme has been recognised nationally and was awarded Best Clinical Innovation Paper at CNSA Congress 2019 and Best Nursing Paper at Blood 2019. "Our programme shares the same mission as the Rosemary Bryant Foundation - to improve health outcomes for all patients through cancer nursing research." Dr Gavin says.
Click
here to read the October 2020 edition of INPractice